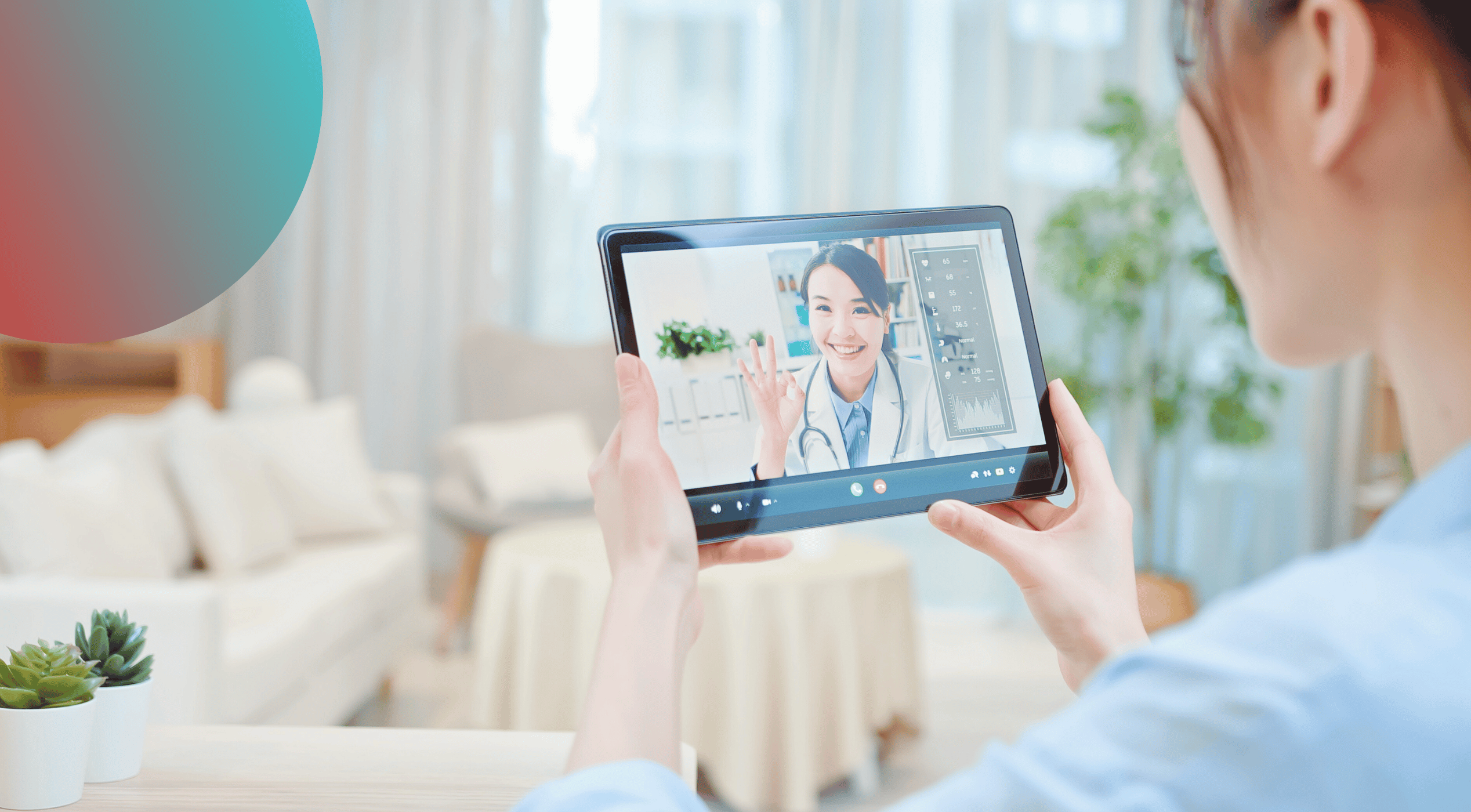
Telehealth in Transition — Navigating Change Beyond the Pandemic
Explore the evolving landscape of telehealth post-pandemic. Learn how policy shifts, payer updates, and compliance considerations impact healthcare providers and coders.
When telehealth use surged during the COVID-19 pandemic, it reshaped how providers delivered care and how patients accessed essential services. But as the public health emergency ended, many of the temporary flexibilities that fueled this growth began to expire — creating uncertainty across the healthcare community.
Today, policymakers continue debating how to balance access, equity, and compliance. And now, with the remaining federal telehealth expansions set to expire at the end of January 2026, the industry is facing another pivotal transition point.
The Legacy of the Pandemic
During the pandemic, telehealth adoption expanded rapidly with:
- Relaxed geographic and originating site restrictions
- Expanded eligible provider types
- Temporary payment parity across many services
These changes allowed millions to receive safe, timely care. Yet most flexibilities were tied to temporary waivers — leaving organizations now navigating shifting requirements as those waivers phase out.

The Current Landscape
As the January 2026 deadline approaches, providers are preparing for several key challenges:
Reimbursement Uncertainty
Medicare’s remaining telehealth flexibilities expire at the end of January 2026, and without legislative action, stricter pre-pandemic limitations may return.
State-by-State Variability
States continue to define licensure, modality requirements, and coverage independently, creating complexity for multi-state organizations and virtual care programs.
Compliance Pressure
Documentation specificity, place-of-service accuracy, and correct modifier use remain high-risk audit areas as payers tighten post-pandemic oversight.
Preparing for the Next Phase
To stay ahead of these shifts, organizations should:
✅ Review payer policies frequently for telehealth-specific coverage changes tied to the coming expiration.
✅ Audit documentation workflows to confirm correct place-of-service and encounter details.
✅ Train providers on proper use of telehealth modifiers (e.g., 95, 93) as requirements change.
✅ Communicate clearly with patients regarding coverage limitations, out-of-pocket expectations, and any changes to virtual care availability.
Telehealth has demonstrated long-term value — but the era of broad, temporary expansion is coming to an end. The next phase will require heightened precision, proactive advocacy, and operational adaptability to ensure access doesn’t erode as policies tighten.
Kaio Coding Solutions™ remains committed to supporting providers and coding professionals through this transition with clarity, confidence, and compliance.
Emily Montemayor

Emily Montemayor, CCS, COC, CPC, CPMA, CMBCS, QMRAC, CPC-I, CPA-EDU, Approved Instructor, is the Founder and President of Kaio Coding Solutions™ and Kaio Learning™, where she empowers healthcare professionals with clarity, precision, and confidence in coding, compliance, and revenue integrity. With over a decade of experience supporting hospitals, providers, and learners nationwide, Emily combines technical expertise with mentorship and innovative education strategies. She is passionate about transforming complex healthcare processes into actionable knowledge and guiding learners to mastery.
Join the
Kaio Luminaries
Sign up for the Kaio Learning™ newsletter to get tips, updates, and early access to courses and webinars — all designed to elevate your skills and career.






.png)
.png)
.png)