
Precision Matters: How Clear Documentation Shapes Compliance and Revenue in 2026
Learn how precise documentation and coding practices in 2026 can maximize revenue, reduce denials, and maintain compliance.
As temporary telehealth flexibilities fade and payer scrutiny increases, accurate documentation and coding have never been more critical. In 2026, clarity and precision in charting will define not only compliance but also revenue integrity, operational efficiency, and audit readiness. Healthcare organizations that prioritize meticulous documentation and coding practices are better positioned to navigate evolving policies and maintain financial stability.
The Importance of Documentation Accuracy
Accurate, complete, and detailed documentation is the foundation of proper coding. Clear notes support correct CPT, HCPCS, and ICD-10 assignments, reducing ambiguity and preventing unnecessary denials. Encourage providers to include specifics about procedures, telehealth visits, modifiers, and clinical rationale to ensure every encounter is fully represented. Inadequate documentation can result in undercoding, lost revenue, or audit findings, while overly vague entries may trigger compliance concerns.
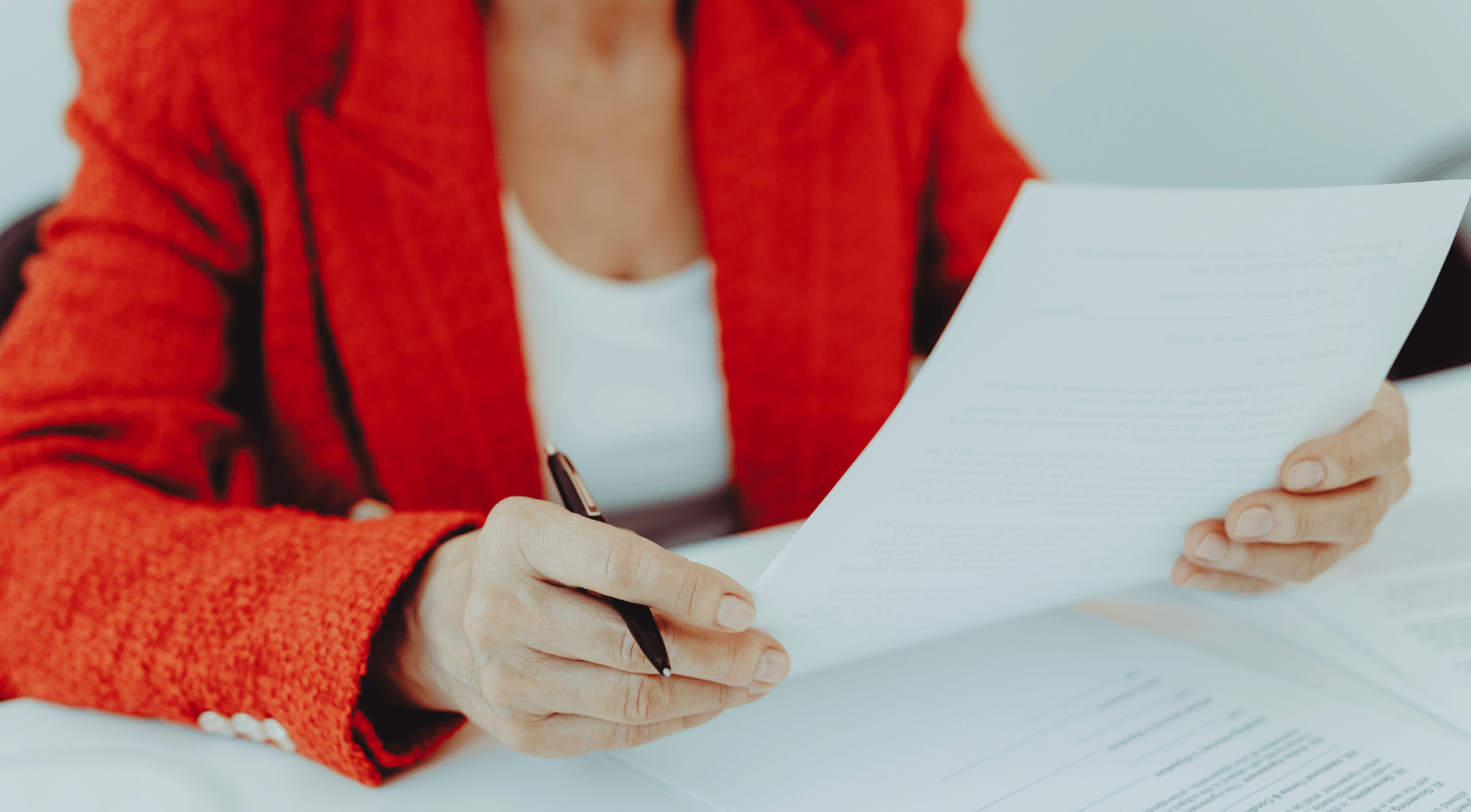
Precision in Coding and Modifier Use
Correct use of procedural and telehealth modifiers (such as 95 or 93) and proper place-of-service reporting is essential. Auditors are increasingly focused on these details post-pandemic, and errors can lead to claim denials, recoupments, or regulatory scrutiny. Coders must stay current on evolving payer policies, documentation requirements, and coding guidelines to maintain accuracy and compliance.
Audit Readiness
Internal audits are an essential tool for maintaining compliance. Regularly reviewing charts, coding decisions, and claim submissions allows teams to identify gaps before payers do. Audit-ready documentation supports defensible claims, ensures accurate reimbursement, and strengthens the organization’s overall revenue integrity program.
Collaboration Drives Success
Successful documentation and coding rely on collaboration between providers, coders, and administrative staff. Establishing clear expectations for documentation and ongoing training reduces errors, improves workflow efficiency, and fosters a culture of accountability. Open communication also helps coders clarify ambiguities and prevent costly mistakes before they reach the claims stage.
Kaio Insight
In 2026, precision in documentation and coding is no longer optional—it’s essential. Clear, accurate records empower coding teams, enhance compliance, and maximize revenue capture, while protecting practices from unnecessary audits and denials.
Learn more about how clarity and precision shape compliance and revenue in 2026 by tuning into our podcast episode “Igniting 2026: Why Clarity and Precision Will Define Documentation & Coding” for practical strategies and expert insights.
Emily Montemayor

Emily Montemayor, CCS, COC, CPC, CPMA, CMBCS, QMRAC, CPC-I, CPA-EDU, Approved Instructor, is the Founder and President of Kaio Coding Solutions™ and Kaio Learning™, where she empowers healthcare professionals with clarity, precision, and confidence in coding, compliance, and revenue integrity. With over a decade of experience supporting hospitals, providers, and learners nationwide, Emily combines technical expertise with mentorship and innovative education strategies. She is passionate about transforming complex healthcare processes into actionable knowledge and guiding learners to mastery.
Join the
Kaio Luminaries
Sign up for the Kaio Learning™ newsletter to get tips, updates, and early access to courses and webinars — all designed to elevate your skills and career.






.png)
.png)
.png)